
During the year, Highmark adjusts the List of Procedures and Durable Medical Equipment (DME) Requiring Authorization . For information regarding authorizations required for a member’s specific benefit plan, providers may:
. For information regarding authorizations required for a member’s specific benefit plan, providers may:

These changes are announced in the form of Special Bulletins and other communications posted on Highmark’s Provider Resource Center (PRC). The most recent updates regarding prior authorization are below:
There’s a new tip sheet posted on the Provider Resource Center that explains how the out-of-area gap exception process works, including the following information:
posted on the Provider Resource Center that explains how the out-of-area gap exception process works, including the following information:
Highmark is experiencing an increased volume of incorrect authorization requests for bilateral musculoskeletal (MSK) procedures. For bilateral procedures, requested units should be in multiples of 2 (e.g., 2, 4, 6, etc.).
To ensure efficient processing of your authorization request for this type of treatment, providers need to include the correct code(s) for bilateral MSK procedures and request units in multiples of 2. This will result in faster approvals for appropriate treatment.
Effective Sept. 30, 2024, nearly 100 codes will be added to the prior authorization list, including codes related to the following procedures and/or treatments:
The codes below will not appear on the Prior Authorization list until the effective date of Sept. 30, 2024. To view the codes now, click here .
.
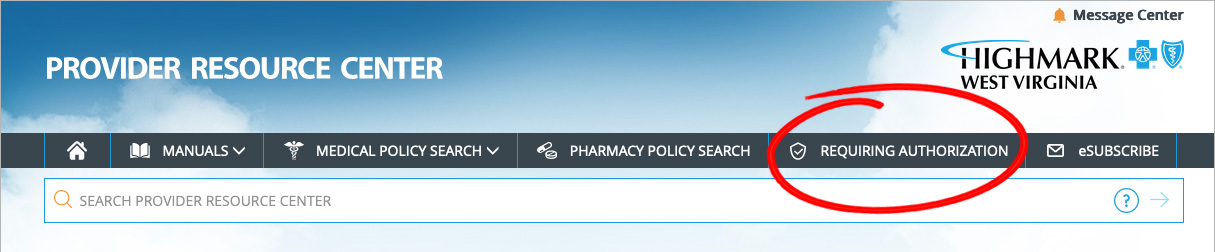
To view the full List of Procedures/DME Requiring Authorization, click REQUIRING AUTHORIZATION in the gray bar near the top of the PRC homepage.
Once redirected to the Procedures/Service Requiring Authorization page, click View the List of Procedures/DME Requiring Authorization under PRIOR AUTHORIZATION CODE LISTS.
Please note that the Highmark member must be eligible on the date of service and the service must be a covered benefit for Highmark to pay the claim.
Availity is the preferred method for:
is the preferred method for: